B cells (B Lymphocytes)
Lymphocytes B and T are the two main types of lymphocytes. B cells work mainly by secreting substances called antibodies into body fluids. Antibodies capture antigens circulating in the blood. However, they do not have the ability to penetrate cells. The task of attacking target cells – either virus-infected cells – or cancer-infested cells is left to T cells or other immune cells (described below).
Each B cell is programmed to produce one specific antibody. For example, one B cell produces an antibody that blocks a virus that causes the common cold, while another produces an antibody that attacks a bacterium that causes pneumonia.
If a B cell encounters a trigger antigen, it causes the growth of many large cells known as plasma cells. Each plasma cell is a specialized antibody factory. Each plasma cell is a descendant of a B cell and produces millions of identical antibodies that are released into the blood. The antibody fits the antigen like a key fits a lock. Some fit very precisely, others more like a pick. But wherever an antibody and an antigen come together, the antibody marks the antigen for destruction. Antibodies belong to a family of large molecules known as immunoglobulins. Different types of antibodies perform different functions in the immune defense strategy.
|
IgA |
Immunoglobulin A has a critical role in immune defense particularly at the mucosal surfaces. IgA is found in many body secretions, including tears, saliva, respiratory and intestinal secretions, and colostrum (the first milk produced by lactating mothers). Very little IgA is present in the serum. IgA is produced by B cells located in the mucous membranes of the body. Two molecules of IgA are joined together and associated with a special protein that enables the newly formed IgA molecule to be secreted across epithelial cells that line various ducts and organs. Although IgG is the most common class of immunoglobulin, more IgA is synthesized by the body daily than any other class of antibody. However, IgA is not as stable as IgG, and therefore it is present in lower amounts at any given time. |
|
IgG |
Immunoglobulin G is the most common class of immunoglobulin. It is present in the largest amounts in blood and tissue fluids. Each IgG molecule consists of the basic four-chain immunoglobulin structure. There are four subclasses of IgG, each with minor differences in its H chains but with distinct biological properties. IgG is the only class of immunoglobulin capable of crossing the placenta; consequently, it provides some degree of immune protection to the developing fetus. These molecules also are secreted into the mother’s milk and, once they have been ingested by an infant, can be transported into the blood, where they confer immunity. |
|
IgM |
Immunoglobulin M is the first class of immunoglobulin made by B cells as they mature, and it is the form most commonly present as the antigen receptor on the B-cell surface. When IgM is secreted from the cells, five of the basic Y-shaped units become joined together to make a large pentamer molecule with 10 antigen-binding sites. This large antibody molecule is particularly effective at attaching to antigenic determinants present on the outer coats of bacteria. When this IgM attachment occurs, it causes microorganisms to agglutinate, or clump together. |
|
IgE |
Immunoglobulin E is made by a small proportion of B cells and is present in the blood in low concentrations. Each molecule of IgE consists of one four-chain unit and so has two antigen-binding sites, like the IgG molecule; however, each of its H chains has an extra constant domain (CH4), which confers on IgE the special property of binding to the surface of basophils and mast cells. When antigens bind to these attached IgE molecules, the cell is stimulated to release chemicals, such as histamines, that are involved in allergic reactions. IgE antibodies also help protect against parasitic infections. |
|
IgD |
Immunoglobulin D molecules are present on the surface of most, but not all, B cells early in their development, but little IgD is ever released into the circulation. It is not clear what function IgD performs, though it may play a role in determining whether antigens activate the B cells. |
T cells (T lymphocytes)
Unlike B cells, T cells do not recognize freely circulating antigens. Rather, their surface has specialized receptors (so-called antibody-like receptors) that recognize fragments of antigens on the surface of infected or cancer cells. T cells participate in immune defense in two main ways: some direct and regulate the immune response; others attack directly infected or cancer cells.
T helper lymphocytes (Th cells) coordinate immune responses by communicating with other cells. Some stimulate nearby B cells to produce antibodies, others call on phagocytes, and others activate other T cells.
Tc cells
Cytotoxic T lymphocytes, also called Tc cells or Tc lymphocytes (Cytotoxic T Lymphocytes - CTLs), perform various tasks. These cells directly attack other cells that carry certain foreign or abnormal molecules on their surface. Cytotoxic T cells are particularly useful in defense against viruses because viruses are often hidden from other elements of the immune system because viruses often multiply inside infected cells. These cells can detect even small fragments of the virus protruding through the cell membrane of a virus-infected cell and attack it to destroy it.
In most cases, T cells can only recognize an antigen if it is carried on the cell surface by its own MHC molecules (major histocompatibility complex). MCH molecules are proteins recognized by T cells when they distinguish between self and foreign. Own MHC molecules create a recognizable scaffold for presenting foreign antigens to T cells.
Although MHC molecules are needed by Tc cells to attack foreign invaders, they pose problems in the case of organ transplantation. Each cell of the body has MHC proteins on its surface, and each person has his or her own set of these proteins. If a Tc lymphocyte recognizes "foreign" MHC molecules on the surface of a cell, which happens in transplants, it will begin to destroy it. Therefore, it is necessary to select organ donors with the set of MH molecules (major histocompatibility complex) that is most similar to the recipient's set. Otherwise, Tc lymphocytes will probably attack the transplanted organ and lead to its rejection.
NK cells
NK cells, or natural killer cells, are another type of white blood cells of the lymphocyte class. Like cytotoxic T cells (LTc), NK cells are armed with granules filled with powerful chemicals. However, while killer cytotoxic T cells look for antigen fragments attached to molecules of "their" MHC, NK cells recognize cells that do not have molecules of "their" MHC. Therefore, NK cells have the ability to attack various types of foreign cells.
Both types of killer cells kill through contact. Assassins attach themselves to their target, turn their weapons on him and trigger a deadly chemical explosion.
Phagocytes and their relatives
 Phagocytes are large white cells that can devour and digest microbes and other foreign particles. Monocytes are phagocytes that circulate in the blood. When monocytes enter the tissues, they transform into macrophages.
Phagocytes are large white cells that can devour and digest microbes and other foreign particles. Monocytes are phagocytes that circulate in the blood. When monocytes enter the tissues, they transform into macrophages.
Specialized types of macrophages are found in many organs: lungs, kidneys, brain and liver. Macrophages perform many functions. Like cleaners, they free the body of used cells and other debris (garbage). They display pieces of foreign antigens so as to attract the attention of the appropriate lymphocytes. They project out an incredible multitude of powerful chemical signals, known as monokines, that are important for the immune response.
Another type of immune system cells are granulocytes. They contain granules filled with powerful chemicals that allow granulocytes to destroy microorganisms. Some of these substances, such as histamine, are also involved in the processes of inflammation and allergy.
One of the granulocytes, the neutrophil, is also a phagocyte; it uses previously stored chemicals to break down and digest microbes. Eosinophils and basophils are other granulocytes that release chemicals from their granules, spraying them onto nearby microbes and harmful cells.
Mast cells are the twins of basophils, except that they are not blood cells. They are found in the tissues: lungs, skin, tongue, mucous membrane lining the nasal cavity and the digestive tract, where they are responsible for allergy symptoms.
A related structure is platelets. These are cell fragments that also contain granules. The function of platelets related to blood cell aggregation, coagulation and wound healing also includes immune activation.
Cytokines
Cytokines are proteins that function as chemical messengers in your immune system. Your immune system is a network with several parts that work together to protect your body from threats, like germs that can make you sick. It contains immune cells that fight invading pathogens (like viruses and bacteria), allergens and other harmful substances that enter your body. Cytokines signal those immune cells to fight the invaders. Even when there’s no threat, cytokines send signals to other cells that keep your immune system functioning.
The components of the immune system communicate with each other by exchanging chemical messengers called cytokines. These proteins are secreted by cells and act on other cells to coordinate an appropriate immune response. Cytokines include a diverse range of interleukins, interferons, and growth factors. Some cytokines are types of chemical switches that turn certain types of immune cells on or off.
Different types of cytokines
Cytokines include different types of proteins that tell immune cells where to go and what to do to keep your immune system functioning correctly.
- Chemokines direct immune cells toward places in your body where they can fight infection.
- Interferons signal cells to put up their defenses against viruses invading your body. In this way, interferons “interfere” in the process that allows viruses to replicate, or make more viruses once they’ve invaded a healthy cell.
- Interleukins get their name from “inter” which means between and “leukocyte,” which is another name for a white blood cell. Originally, scientists thought that leukocytes alone released interleukins and only relayed messages to other leukocytes. But now we know that cells other than leukocytes release these proteins. Also, interleukins can relay messages between cells that aren’t leukocytes.
- Tumor necrosis factor (TNF) helps regulate inflammation in your body. TNF also signals to immune cells that kill tumor cells.
- Colony-stimulating factors CSF signals hematopoietic stem cells to develop into specific cell types. Hematopoietic stem cells (HSC) are precursor cells that give rise to all blood cell types: white blood cells, red blood cells and platelets. These changes take place during a process called hematopoiesis. For example, granulocyte-colony stimulating factor (G-CSF) signals an HSC to become a white blood cell called a neutrophil. Neutrophils help fight infection.
- Lymphokines – produced by lymphocytes, a type of white blood cell.
- Monokines – produced by monocytes, a type of white blood cell.
One of the cytokines, interleukin 2 (IL-2), triggers the production of T cells by the immune system. The immune-stimulating properties of IL-2 have traditionally made it hopeful in the treatment of a number of diseases. Clinical trials are underway testing their benefits in other diseases such as cancer, hepatitis C, HIV infection and AIDS. Other cytokines are also being investigated for their potential therapeutic benefits and clinical applications.
Other cytokines chemically attract particular types of cells. These so-called chemokines are released by cells at the site of damage (injury) or infection and call other immune cells to the site to help repair the damage and fight off invaders. Chemokines often play a key role in inflammation and are promising targets for new drugs that regulate the immune response.
The complemment system
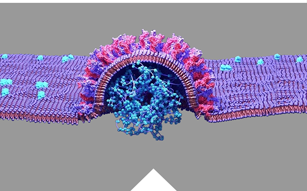
The complement system contains approximately 25 proteins that work together to "complement" the action of antibodies in destroying bacteria. Complement also supports the body's release from antigen-antibody complexes. Complement proteins, which cause blood vessels to dilate and cause their permeability, are involved in the development of redness, swelling, pain, increase in temperature and loss of function that characterize the inflammatory response.
Complement proteins circulate in the blood in an inactive form. When the first complement protein is activated – typically by an antibody that locks with an antigen – a domino effect is triggered. Each component (takes) contributes to a precise chain of steps known as the complement cascade. The end product is a cylinder that sticks into the cell wall, creating a hole (hole) in it. Fluids and particles flow in and out through it into the cell, which swells (buzzes) and bursts. Other components of the complement system make bacteria susceptible to phagocytosis and/or attract other cells to the region.